Resources
Understanding the
Neuropsychological Evaluation
A neuropsychological evaluation is a detailed assessment of memory, attention, reasoning, language, executive functioning, and emotional health. Many people arrive feeling unsure of what to expect. These guides help answer common questions and reduce uncertainty.
What to Expect During a Neuropsychological Evaluation
Learn how the evaluation is structured and what each part of the process is meant to uncover. This overview explains how the interview, testing, and feedback session work together to provide a complete understanding of cognitive functioning.
How to Prepare for Testing
Simple planning can make the day smoother. This includes getting adequate sleep, taking prescribed medication as usual unless instructed otherwise, bringing glasses or hearing aids, and eating beforehand. Patients are encouraged to arrive in comfortable clothing and plan for breaks as needed.
Understanding Your Results
A clear explanation of how findings are interpreted and how strengths and weaknesses are identified. This section helps patients understand what a percentile means, how cognitive profiles are described, and how results relate to real life.
Information on Common Conditions
The brief summaries below describe some of the most common reasons adults and older adults are referred for a neuropsychological evaluation. They are not meant to provide diagnoses on their own. Instead, they offer context so you can better understand why testing may have been recommended.

Mild Cognitive Impairment (MCI)
- Mild Cognitive Impairment is a condition in which a person has more difficulty with thinking or memory than would be expected for age, but daily activities such as dressing, basic self care, and simple household tasks remain mostly independent. It is often described as an “in between” state that falls between typical aging and dementia.
- Common concerns include repeating questions, losing track of conversations, misplacing items more often, or needing more time to process information. Some people primarily notice memory changes. Others may have more difficulty with attention, planning, word finding, or visual spatial skills.
- MCI can have many possible causes. In some cases it represents an early stage of a neurodegenerative condition such as Alzheimer’s disease. In other cases it is related to mood, sleep, medical illness, vascular risk factors, or the effects of medication. Not everyone with MCI progresses to dementia, and some people remain stable for many years.
- A neuropsychological evaluation helps to clarify whether changes are consistent with MCI, which cognitive abilities are most affected, and whether the pattern raises concern for an underlying neurodegenerative process or suggests other contributing factors such as anxiety, depression, or medical issues. This information can guide monitoring, lifestyle changes, and medical follow up.
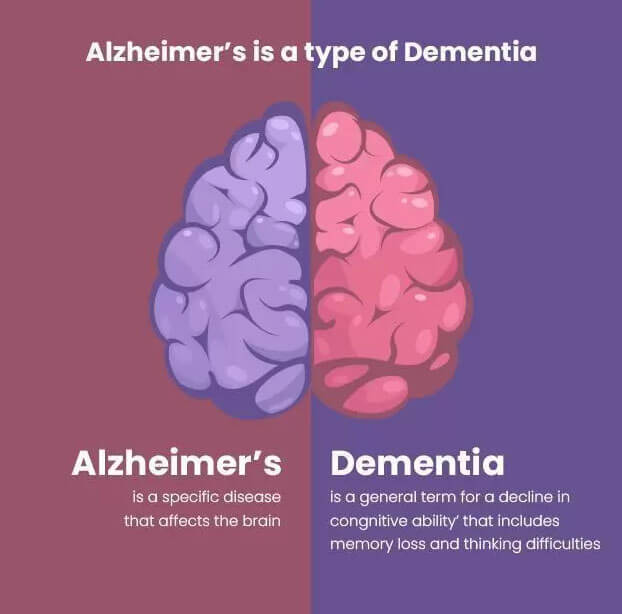
Alzheimer’s Disease and
Related Dementias
- Alzheimer’s disease is the most common cause of dementia. It is characterized by gradual decline in memory and other cognitive abilities that interferes with independence in daily life. People may have increasing trouble recalling recent events, managing finances, following multi step tasks, keeping track of appointments, or navigating in familiar places. Over time, changes in language, problem solving, judgment, and behavior may also appear.
- “Related dementias” include other conditions that can cause progressive cognitive decline, such as vascular dementia, dementia with Lewy bodies, frontotemporal dementia, and mixed dementias in which more than one process is present. Each has its own typical pattern of changes. For example, vascular causes often produce more uneven or stepwise changes, while Lewy body disease may involve prominent fluctuations, visual hallucinations, and changes in attention or movement.
- Neuropsychological testing plays an important role in this area. It helps document whether a person meets criteria for a major neurocognitive disorder, identifies which cognitive abilities are most affected, and distinguishes patterns that are more suggestive of Alzheimer’s disease versus other causes. Test results are often combined with medical history, imaging, and sometimes biomarkers to support diagnosis, treatment planning, and decisions about safety and support.

Movement Disorders such as Parkinson’s Disease
- Parkinson’s disease and other movement disorders are often thought of as conditions that primarily affect movement. However, they can also affect thinking, mood, and behavior. Many people with Parkinson’s experience changes in attention, processing speed, executive functioning, and visual spatial skills. Memory can also be affected, although the pattern often differs from Alzheimer’s disease.
- Some individuals develop Mild Cognitive Impairment related to Parkinson’s disease, while others go on to develop Parkinson’s disease dementia over time. Common concerns include slowed thinking, difficulty multitasking, trouble keeping track of complex information, and changes in planning or problem solving. Visual spatial difficulties, such as judging distances or navigating in new environments, are also common and may impact driving or daily tasks.
- A neuropsychological evaluation helps to identify and monitor these cognitive changes. It can clarify which abilities remain strong, which are beginning to decline, and how these changes are affecting daily functioning. This information can guide treatment decisions, rehabilitation strategies, safety planning, and support for both the person with Parkinson’s and their caregivers.
Attention Difficulties and A-D/HD in Adults

- Attention Deficit Hyperactivity Disorder can persist into adulthood, even if it was never formally diagnosed in childhood. In adults, symptoms often look different than they do in children. People may describe chronic distractibility, difficulty staying organized, trouble finishing tasks, frequent procrastination, or a tendency to act quickly without thinking through consequences. These patterns can affect work, relationships, education, and daily responsibilities.

- However, attention difficulties in adults are not always due to A-D/HD. Anxiety, depression, sleep problems, chronic pain, trauma history, and certain medical or neurological conditions can all interfere with focus and mental efficiency. For some individuals, longstanding personality traits or high levels of stress can also play an important role
- Neuropsychological assessment helps to clarify whether an adult’s attention and executive functioning difficulties are consistent with A-D/HD or are better explained by other factors. Testing examines sustained attention, working memory, processing speed, planning, and self-regulation in the context of the person’s history and current emotional state. The goal is not simply to label but to understand the pattern of strengths and weaknesses and to guide reasonable recommendations, which may include behavioral strategies, environmental supports, psychotherapy, and in some cases a medical discussion about stimulant or non-stimulant medications.
Concussion and Post
Concussive Symptoms
- A concussion is a mild traumatic brain injury, often caused by a fall, sports injury, accident, or impact to the head. Most people recover within a few days to a few weeks, and symptoms are usually temporary. However, a subset of individuals experience symptoms that persist for months or longer. When symptoms last beyond about three months, this may be described as post concussive syndrome.
- Common symptoms can include headaches, fatigue, dizziness, sensitivity to light or noise, trouble concentrating, memory difficulties, slowed thinking, irritability, anxiety, or changes in sleep. These symptoms can significantly affect work, school, driving, and daily life, even when routine brain scans appear normal. Persistent symptoms are often influenced by a combination of physical, cognitive, and emotional factors rather than by ongoing structural brain damage alone.
- Neuropsychological evaluation helps to clarify which cognitive skills are affected after a concussion and how those changes interact with mood, stress, sleep, and pain. Testing can provide a baseline for recovery, identify areas that would benefit from cognitive rehabilitation or workplace or academic accommodations, and offer practical strategies for managing daily tasks while symptoms improve. For individuals with prolonged difficulties, this type of evaluation can also help distinguish post concussive effects from other conditions such as depression, anxiety, or unrelated cognitive disorders.
Functional Cognitive Disorder
- Functional Cognitive Disorder involves real and often distressing difficulties with memory, attention, or thinking that are not caused by neurological disease. These symptoms can feel similar to early dementia, yet brain scans and neurological examinations are typically normal.
- Many individuals with functional cognitive symptoms experience high levels of stress, anxiety, trauma history, sleep disturbance, burnout, or chronic pain. These factors can interfere with the brain’s ability to process information efficiently, leading to forgetfulness, mental fatigue, difficulty concentrating, or a sense of cognitive overwhelm. The symptoms are genuine and can significantly impact daily life.
- A neuropsychological evaluation helps determine whether cognitive complaints reflect a functional pattern rather than a neurodegenerative or medical condition. The goal is to provide clarity and reduce fear by explaining how emotional or physiological factors affect cognitive performance. Treatment often focuses on targeted strategies, psychotherapy, stress management, and lifestyle supports that help improve daily functioning and restore confidence.
Vascular Cognitive
Impairment and Stroke
- Vascular Cognitive Impairment refers to changes in thinking and memory caused by reduced blood flow to the brain. This may occur gradually due to small vessel disease or more suddenly after a stroke. People may notice slowed thinking, difficulty planning or organizing, changes in attention, or challenges with problem solving, even if memory remains relatively strong.
- A stroke can affect thinking in different ways depending on the area of the brain involved. Some individuals have trouble understanding language, while others may experience changes in mood, behavior, or visual spatial abilities.
- A neuropsychological evaluation helps identify which specific cognitive abilities have been affected and how these changes may influence daily functioning. This information supports treatment planning, rehabilitation, decisions about independence, and long term risk management, including attention to vascular health factors such as blood pressure, cholesterol, diabetes, and lifestyle.
Cognitive Symptoms Associated with Long COVID
- Some individuals continue to experience thinking and memory difficulties after recovering from COVID infection. These symptoms may include trouble concentrating, slowed mental processing, forgetfulness, difficulty multitasking, mental fatigue, or challenges completing tasks that previously felt effortless. These changes are sometimes referred to as post COVID cognitive symptoms or informal terms such as brain fog.
- Research suggests that these symptoms may be influenced by a combination of factors such as inflammation, disrupted sleep, fatigue, mood changes, altered stress response, and the body’s prolonged recovery process. Although symptoms can be frustrating and may interfere with work, school, or daily responsibilities, many people improve over time with appropriate support.
- A neuropsychological evaluation helps clarify which cognitive areas are affected and how these changes relate to daily life. The evaluation also helps distinguish long COVID symptoms from other conditions such as depression, anxiety, post concussive effects, or early neurodegenerative illness. Recommendations typically focus on pacing strategies, cognitive rehabilitation, environmental supports, sleep optimization, and coordinated medical care.